Flu epidemics are a yearly recurring event, caused by the mutational strength of the virus that causes the disease: influenza. Because of the high tendency to mutate, and therefore evade our immune system and the drugs we develop, scientists have been looking at new ways to get rid of the influenza virus. A new method focuses at boosting the body's response, instead of targeting the virus itself. Two new lead compounds that are currently being tested showed high efficacy against three strains of influenza, one of them being the famous viral strain that caused a pandemic in 1918, killing between 50 and 100 million people worldwide. The flu currently kills about half a million people in the world each year. A novel protection mechanism could bring down the number of deaths, as well as rendering the need for yearly flu vaccines unnecessary.
According to the scientists, their potential new drugs upregulate the production of a protein called REDD1, that works as an infection-fighting agent. By upping the amount of REDD1, experiments with the infection of cells showed that the treatment was able to fight off the influenza. The researchers showed that the protein forms a barrier for viral infection, something that had not been shown before. REDD1 has an interesting duality, because it was also found to be active in regulating cell proliferation, which could be important to prevent cancer. Because no testing in animals or humans has been done, it will take many more years before a potential drug based on activating REDD1 can be put on the market.
According to the scientists, their potential new drugs upregulate the production of a protein called REDD1, that works as an infection-fighting agent. By upping the amount of REDD1, experiments with the infection of cells showed that the treatment was able to fight off the influenza. The researchers showed that the protein forms a barrier for viral infection, something that had not been shown before. REDD1 has an interesting duality, because it was also found to be active in regulating cell proliferation, which could be important to prevent cancer. Because no testing in animals or humans has been done, it will take many more years before a potential drug based on activating REDD1 can be put on the market.
The influenza virus is mainly characterized by two proteins on the outer layer of the viral wall: hemagglutinin (H) and neuraminidase (N). These proteins vary in their structure from strain to strain and make up the specific name of the viral strain. The famous 1918 viral strain is called H1N1, while the outbreak of 'bird flu' in 2006 was caused by H5N1. H1N1 has reared its head multiple times, with the last outbreak being the 'swine flu' of 2009.
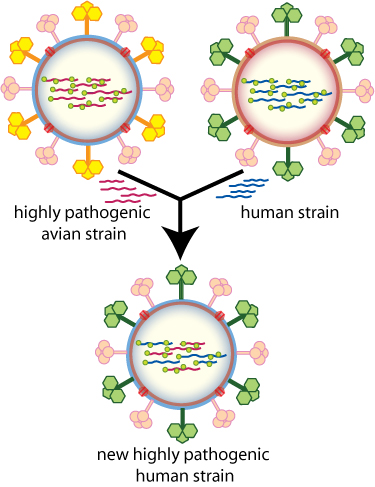
Viral strains have the ability to mutate their H and N proteins, so that new rearrangements are able to infect humans again each year. The mutations are stimulated by the body's immune response, which renders an "old" strain to be less effective with infecting cells. The pressure to mutate causes new outbreaks of flu every year, and causes major panic ever so often, when a new, highly contagious, strain is found that could possibly cause a widespread pandemic. Bird flu and swine flu were examples of this, although their spread was halted prematurely. New influenza subtypes can also arise by combining two viral strains. The result is a hybrid form to which the body has not been able to build up protection yet.
Developing potent new anti-influenza drugs may become even more relevant soon, as scientists have discovered that a total of only five mutations in just two genes can make the H5N1 strain much more deadly. Currently, it's fairly limited in spreading among humans, but the mutations that were induced by the researchers show this may change. Five genetic mutations in order to significantly increase in deadliness is not a lot. Stacking five mutations on top of each other is very rare, but as viruses readily mutate and exists by the billions, it suddenly becomes a lot more likely. The scientists did not elaborate on the chance that this set of mutations will appear in the wild.


No comments:
Post a Comment